Social Determinants of Health
This article was written by Lisa Miller.
This blog is the second and final part of our research proven SDOH (Social Determinants of Health) strategies for your hospital.
You can read the first part here.
Introduction
In order to address the root causes of poor health and high hospital utilization, health systems have begun to form collaborative SDOH initiatives within their communities.
Healthcare leaders recognize the vital role a patient’s social needs play, alongside medical care, to achieve the best possible outcomes.
Poverty is a key predictor of poor health. As such, efforts to alleviate root causes including unemployment, poor education, language barriers, community violence and safety within communities are all key targeted areas for healthcare community involvement.
Poverty is a key predictor of poor health. Efforts to alleviate root causes, i.e. unemployment, poor education and safety, are essential. #SDOH Click To Tweet
Furthermore, the growth of population health programs has increased, and hospital leaders are seeking to identify proven strategies to improve the overall health within their communities. Stakeholders include healthcare and community organizations, federal, state and local agencies and philanthropic entities working in partnership to find actionable solutions.
One such “call to action” is the Healthcare Anchor Network [1], comprising 50 hospitals and health systems. The following is an excerpt from their website:
“The Healthcare Anchor Network is a health system-led collaboration that helps participants to more rapidly and effectively advance an Anchor Mission approach within their institution, in authentic partnership with the communities they serve, and across the healthcare sector… Hospitals and health systems are critical local economic engines and mission-driven organizations inextricably linked to the long-term well-being of those we serve—because of this, we as healthcare leaders, are uniquely positioned and incentivized to play a more active role in supporting our local economies. We have an opportunity and obligation to improve health and well-being outcomes in the communities we serve and confront economic and social instability in our nation that remain obstacles to that goal.”
Multiple inequities exist within communities (relating to race, immigration status, sexual orientation, etc). In addition, there are varying needs based on issues such as geographic location (i.e. urban vs rural, climate variances, access to healthcare facilities and public transportation, etc).
While numerous efforts have been made by hospitals and health systems to develop various community programs, many are fragmented and lack funding. In reviewing the current literature, it is evident that a focused strategic approach must select one or two identified community needs and work to implement programs to address those specific needs.
Partnerships with community organizations and funding opportunities must be explored prior to creating the strategic map.
Hospital success stories
In our previous blog, we explored successful strategies around food insecurity, social support and social isolation, transportation and housing instability.

Here, we will focus on the following social needs projects developed by hospitals and health systems in conjunction with community partners, which include:
- Neighborhood and physical environment risk factors.
- Language barriers and literacy.
- Education and economic stability.
- Safety, violence and incarceration.
1. Neighborhood and physical environment risk
Examples of effective strategies are given below:
(i) Medical and legal assistance with poor housing environment.
In poverty stricken neighborhoods, patients may live in poor housing with no recourse to improve their environment. Johns Hopkins Medicine’s PROJECT HEAL [2] is a medical/legal assistance program, developed to assist patients with poor housing conditions (mice, roaches, mold, lead, etc), landlord/tenant problems (including evictions and security deposits), school issues, custody problems/child support, termination of public benefits and so on.
(ii) Benefits of medical/legal partnerships are documented in [3]:
‘’The medical-legal partnership is a collaborative intervention that embeds civil legal aid professionals in health care settings to address seemingly intractable social problems that contribute to poor health outcomes and health disparities. More than three hundred health care organizations are home to medical-legal partnerships. ….Financing and commitment from health care organizations are key considerations for sustaining and scaling up the medical-legal partnership as a health equity intervention.
(iii) Maternal health screening for environmental stressors (ie, mental health, domestic violence):
“The Harriet Lane Clinic (HLC) has dedicated staff to meet with young mothers of newborns to screen for postpartum depression, intimated partner violence and other significant family stressors, which are all factors that are directly linked to poor health and developmental outcomes for infants.” [4]
(iv) Chronic health conditions-environmental factors/pediatric asthma
Boston Children’s Hospital Community Asthma Initiative (CAI) is a program designed to reduce health disparities among children with asthma. It includes a home environment assessment and a plan for remediation. [5]
2. Language barriers and literacy
(i) In one case study, language barriers contributed to a parent’s discomfort with discharge instructions at the Children’s Hospital of Montefiore, Bronx NY. After reviewing the root causes, Montefiore determined that the absence of comprehensive screening for a patient with multiple social needs (such as homelessness, language barriers, lack of transportation) was the cause. A program was initiated to deliver improved SDOH screening and post discharge follow-up care. [6]
(ii) Jefferson Health/Philadelphia, PA
In a further study, in partnership with the Philadelphia Collaborative for Health Equity, Jefferson Health received a $3.1 million gift from the Wyss Foundation to build a South Philly Refugee and Immigrant Wellness Center: The Hansjörg Wyss Wellness Center.
The center “will serve as the hub of Jefferson’s clinical and educational outreach activities for the city’s southern neighborhoods and establish primary care and social services to all members of the community — regardless of health insurance or citizenship status.” [7]
3. Education and economic stability
Effective strategies in this area of SDOH include:
(i) Jefferson Health/ Philadelphia Collaborative for Health Equity -Community Assistance with Employment through the development of the Steven H. Korman Center for Community Engagement
“The Steven H. Korman Center for Community Engagement helps disadvantaged and underemployed Philadelphians secure in-demand jobs in healthcare, providing career training and support for GED attainment, comprehensive case management, and job placement. The center currently offers a community health worker certification with peer support specialist training, certified nursing assistant training, and certified medical assistant programs. Philanthropic support will strengthen our efforts to provide educational and career opportunities for our most vulnerable neighbors, helping us achieve our mission to improve lives by placing more individuals on the path to success.” [8]
a) Rush University Medical Center (as a member of the Healthcare Anchor Network) utilizes the Anchor Mission Playbook [9] in their employment practices. These practices include:
- Inclusive local hiring strategies.
- Hire and develop talent.
- Hire locally and create sustainable career pathways for entry level employees.
- Utilize local labor for capital projects.
b) Montefiore Medical Center, Bronx, NY- Maintains a school embedded health program: [10]
“The Montefiore School Health Program (MSHP)—the largest and most comprehensive school-based health program in the country—provides coordinated primary and preventive healthcare to public elementary, middle and high school students throughout the Bronx… Our community-wide public health programming is designed to educate, empower and support students, parents and families to develop healthy habits and take responsibility for improving their overall health and wellness”
4. Safety, violence and incarceration
In November 2018, the American Public Healthcare Association deemed violence a public health crisis. [11]
“Violence disproportionately affects vulnerable populations such as women, children, lesbian, gay, bisexual, transgender, questioning, and intersex individuals, and those living in poverty, among others.” [12]
American Academy of Family Physicians
Examples of initiatives related to this area include:
(i) Incarceration – increase in healthcare utilization.
The Camden Coalition of Healthcare Providers designed a program which integrated health care and criminal justice data as a screening tool to identify vulnerable populations at risk for readmissions. [13]
“Coalition researchers found that a small number of Camden residents have an enormous and disproportionate ‘’……impact on the health care and criminal justice sectors, neither of which is designed to address the underlying problems they face: housing instability, inconsistent or insufficient income, trauma, inadequate nutrition, lack of supportive social networks, mental illness, and substance abuse disorders. These unaddressed social determinants of behavior appear to drive a cycle of repeated arrests and hospitalizations.”
“The most important finding from this study may be that there is enormous value in fostering collaborative data sharing among agencies. By highlighting the power of cross-sector integrated data to unlock key insights into at-risk populations, this study showcases the potential of cross-sector collaboration to provide better outcomes in public safety and public health.”
(ii) Grady Memorial Hospital, Atlanta, GA implemented a workplace violence program.
‘’Grady Health’s workplace safety and violence initiatives have made an enormous impact on the lives, health and well-being of their employees, patients and visitors to their hospital campus.” [14]

Conclusion
These are just some of multiple and varied initiatives that hospitals and health systems have undertaken to improve the health and well-being of their patients:
- Hospitals utilize population health management tools and screen patients in primary care and facility settings to identify social needs.
- In addition, they are developing community partnerships and training staff to engage in compassionate conversations with their patients regarding their living environments and the stressors in their lives.
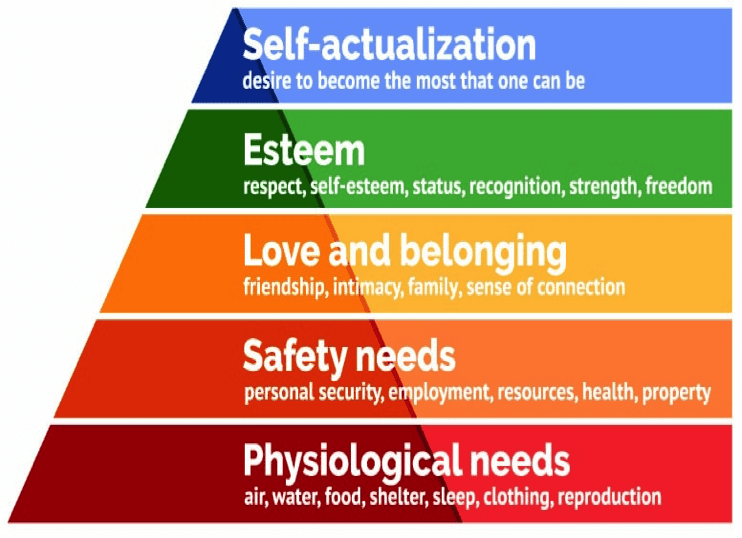
SDOH and Maslow’s Hierarchy of Needs
The social determinants of health can be directly correlated with Abraham Maslow’s Hierarchy of Needs.
As healthcare providers, we have an obligation to provide quality medical care, and open our eyes to the environments and stressors which inhibit our patients’ recovery and clinical outcomes.
As healthcare providers we must open our eyes to the environments and stressors which inhibit patient recovery and clinical outcomes. Click To Tweet
Clean air and water, access to healthy food and safe living conditions are the basic physiological needs identified by Maslow. Personal security, employment, and good health are the next tier of human needs.
Hospitals and healthcare staff can develop patient and family relationships, build trust, and through community interaction provide a sense of connection for our patients.
As we develop the patient-provider relationship, we show our patients respect, help them build self-esteem, and strengthen our communities.
In doing so, we extend our partnership beyond our medical excellence to assist with other social needs within our patient’s lives.
Maslow’s Hierarchy of Needs
References:
[3] Regenstein M, Trott J, Williamson A, Theiss J. Addressing Social Determinants of Health through Medical-Legal Partnerships. Health Aff (Millwood). 2018; 37(3):378–385. doi:10.1377/hlthaff.2017.1264
[5] Woods, ER, Bhaumik U, Sommer SJ, et al; Community Asthmas Initiative to Improve Health Outcomes and Reduce Disparities Among Children with Asthma. CDC- Morbidity and Mortality Weekly Report Supplement 2016; 65(1); 11–20. https://www.cdc.gov/mmwr/volumes/65/su/su6501a4.htm
[6] Yonit Lax, Maria Martinez and Nicole M. Brown; Social Determinants of Health and Hospital Readmission; Pediatrics 2017; 140; DOI: 10.1542/peds.2017-1427 https://pediatrics.aappublications.org/content/pediatrics/140/5/e20171427.full.pdf
[8] https://p-che.org/get-involved/current-efforts/
[9] Ubhayakar S, Capeless M, Owens R, Snorrason K, Zuckerman D. Anchor Mission Playbook [Report]. Chicago, IL and Washington, DC: Rush University Medical Center and the Democracy Collaborative; August 2017. https://www.rush.edu/sites/default/files/anchor-mission-playbook.pdf
[10] https://www.montefiore.org/school-health-program
[12] [https://www.aafp.org/about/policies/all/violence-public-health-concern.html
[13] Milgram, Anne, Jeffrey Brenner, Dawn Wiest, Virginia Bersch, and Aaron Truchil. Integrated Health Care and Criminal Justice Data — Viewing the Intersection of Public Safety, Public Health, and Public Policy Through a New Lens: Lessons from Camden, New Jersey. Program in Criminal Justice Policy and Management, Harvard Kennedy School, April 2018. https://www.hks.harvard.edu/sites/default/files/centers/wiener/programs/pcj/files/integrated_healthcare_criminaljustice_data.pdf
[14] https://www.aha.org/system/files/2018-11/grady-workplace-case-example.pdf
[15] Miriam Ryvicker and Sridevi Sridharan; Neighborhood Environment and Disparities in Health Care Access Among Urban Medicare Beneficiaries With Diabetes: A Retrospective Cohort Study; The Journal of Health Care Organization, Provision, and Financing;2018 Volume 55: 1–12; https://doi.org/10.1177/0046958018771414
[16] Butkus R, Rapp K, Cooney TG, et al, for the Health and Public Policy Committee of the American College of Physicians. Envisioning a Better U.S. Health Care System for All: Reducing Barriers to Care and Addressing Social Determinants of Health. Ann Intern Med. 2020; 172:S50–S59. doi: https://doi.org/10.7326/M19-2410